INTERVIEW
Digital transition is inevitable and necessary for healthcare systems if they do not want to be left behind. Population’s digital skills are usually in the spotlight of the debate, but less often healthcare professionals’ digital abilities are discussed. Andreas Charalambous, president of the European Cancer Organisation (ECO) and an expert in oncology nursing, talks to us about health workforce’s challenges in digital transition and technology-based interventions for cancer care.
Question: We know that health literacy and digital health literacy contributes to improve people’s quality of life. How can healthcare professionals’ level of digital health literacy affect the healthcare system and patients’ lives?
Answer: Having digital health literacy skills means possessing the ability to properly understand and use medical information to influence decision-making on health issues. Digital health literacy is one of the main reasons that explains why digital health cannot reach its full potential in our days. We’re living in a digital age where health information does not only come from medical centres and professionals, but also from the Internet, specific health apps, etc. It is essential that individuals hold the ability to critically assess this information, since the way they will choose to use it might impact their lives.
When levels of digital health literacy are low among population, users cannot fully exploit the resources around them to influence their decision-making process and harness the opportunities technology offers. The same happens with healthcare professionals. Developing these skills allows the health workforce to use available information and technology to its full scope. In general, levels of digital health literacy in Europe are far from the desired levels. People need to be able to manage all this information and it is critical to increase digital health literacy skills for this purpose.
We’ve mapped the existing digital training programmes for healthcare professionals across 14 EU member states and, for example, only 4.2% of these programmes address cancer care.
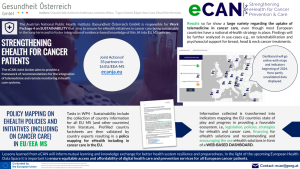
One priority at the European level is to improve and implement a digitalised healthcare system. Are healthcare professionals prepared or trained to assume a European digitalised healthcare system?
It is fantastic that the European Commission is committed to digital transition, but I’m pretty much confident that the health workforce is not well prepared for a digitalised healthcare system. In a EU project that I coordinate, TRANSiTION, we aim to build healthcare professionals’ digital skills. We’ve mapped the existing digital training programmes for healthcare professionals across 14 EU member states and, for example, only 4.2% of these programmes address cancer care. That means there is a lot to be done to better prepare the workforce, build digital competences and make them master this digital transition. Definitely, we are not there yet.
Are digital health literacy skills akin among the workforce across Europe?
There are inequalities when it comes to digital skills among the workforce in Europe. There are countries without digital skills training programmes at all, and I do think this is unacceptable. Without these training programmes being in place, workforce cannot learn basic digital skills and will not be able to uptake more complex tasks. For example, you cannot operate AI machine learning or advanced digital image diagnosis. We need to start from the basic, and then move on from there.
Do you think there are examples of good practices that can be a touchstone to look at?
We have been looking at the Digital Skills Gap Index (DGPI), that identifies and evaluates the factors that underpin the pillars of digital strength, resilience, and responsiveness in different countries and sectors. In Europe, Scandinavian countries, along with The Netherlands and Germany show better performance than some other Southern European countries, such as Greece, Croatia, Slovakia and Hungary.
In all these countries, the presence of institutions that upgrade digital skills, the responsiveness of the educational system and economy and the governmental support they get remain key aspects to improve digital skills among professionals.
At the high-level meeting for cancer prevention and care held in Barcelona in September, you stated that “we need to emphasise and work within the spectrum of multidisciplinary and multiprofessional teams to address cancer care”. Which kind of professionals should be part of this multidisciplinary approach towards cancer care?
A multidisciplinary team consists of medical specialists and other professionals that contributes to fully address what the patient requires. The needs of the patient are very dynamic, and they evolve from diagnosis to treatment, after treatment, as survivors, etc. In this sense, the composition of the team should also change and reflect the needs of the patient, starting with medical oncologists, radiation oncologists, cancer nurses, physiotherapists, nutritionists, occupational therapists and so on. Then you can add other professionals to cover the social aspects and spiritual needs of the patient.
I do think that people developing these apps have understood the important role informal caregivers play in the continuation of care at home and the empowerment they can place into the patients.
In one of your latest publications as an editor (Informal Caregivers: From Hidden Heroes to Integral Part of Care), there is a chapter about the use of information and communication technology by informal caregivers. Can this technology help caregivers to improve their performance? How?
Cancer is, by definition, a social disease. In this context, it is never, and it has never been only the patient on the receiving end. It is always the patient and plus. That plus is usually a caregiver that used to be a family member, but nowadays they can be significant others who are not relatives. Caregivers usually work in groups of two or more and when a patient i trained to use a telemonitoring application for home, such as the eCAN pilot projects, then the informal caregiver is trained to use the app as well. It is becoming much more frequent to include patients and caregivers’ views in these apps. I do think that people developing these apps have understood the important role informal caregivers play in the continuation of care at home and the empowerment they can place into the patients. They become more confident to use this technology.
As healthcare systems acknowledge the essential role of caregivers and how technology can help them to better care for their loved ones, it is becoming more evident that caregivers also need to have the digital health literacy skills. We shouldn’t forget that the caregiver should receive training as well.
Can you develop a bit more the concept of cancer as a social disease?
When you have a heart disease, it is basically you who experience the impact and manifestation of this disease. But when you have cancer, it affects you, your immediate family, your community. The impact of cancer is greater compared to other diseases. Cancer is unique because suffering or experiencing the manifestations of cancer is not confined within the person, it touches the people next to you. That is why we call it a social disease. By no means cancer cannot happen in a social vacuum, the person almost never experiences it alone, and for some reason cancer collects around the person a supportive network, not only immediate family but also significant others.
You have also researched the effects on anxiety and quality of life of breast cancer patients. Taking your results into account, in which ways could technology-based interventions help patients to improve their quality of life?
Depending on the context in which these technologies are applied, there are many ways that can contribute to improve patients’ lives. We have used virtual reality in patients that undergo different kinds of chemotherapy in the day hospital units. They are sitting in a chair for a considerable amount of time, so virtual reality was used as a distraction technique that took the patients away from the stressful environment of the daily unit, from the actual chemotherapy dripping into their bodies. Virtual reality broke their stressful routine of receiving treatment by engaging the patient in a relaxing and interactive environment that patients could enjoy without moving from the chair, through teleporting.
We have also used other methods, such as progressive muscle relaxation and guided imagery scripts that also worked, and we did this in the patients’ environment, so they learn how to do it themselves. We empowered the patient to do it.
As you know, our pilot projects are trying to identify the differences between implementing technology-based interventions and face-to-face interventions in cancer care. Do you think this study can contribute to the research field?
One of the pilots is here in Cyprus, by applying the eCAN project in clinical practice we will be able to demonstrate if technology-based training is as efficient, lower or superior to face-to-face training. I do think that the results coming out for eCAN will contribute to the body of evidence in the field.
![]() Co-funded by the European Union. Views and opinions expressed are however those of the author(s) only and do not necessarily reflect those of the European Union or HaDEA. Neither the European Union nor the granting authority can be held responsible for them.
Co-funded by the European Union. Views and opinions expressed are however those of the author(s) only and do not necessarily reflect those of the European Union or HaDEA. Neither the European Union nor the granting authority can be held responsible for them.

 The Photo Project
The Photo Project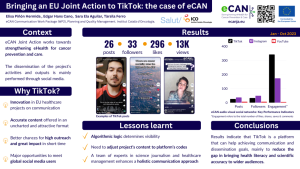
 Pexels (Thirdman)
Pexels (Thirdman)