INTERVIEW
In the COVID-19 pandemic, we witnessed the constant interaction between the scientific and political worlds. While these realities are interrelated and interdependent, they have not always been able to reach consensus on the best ways to improve our health. In the face of today’s major health challenges (climate change, antimicrobial resistance, rising cancer rates, etc.), it is imperative that both communities work together for addressing the mentioned challenges.
Precisely one entity that builds bridges between these groups is the European Observatory on Health Systems and Policies (OBS), which has been celebrating its 25th anniversary in 2023. With the elections for the European Parliament around the corner, Dimitra Panteli and Florian Tille, both from OBS, tell us about how they interact with the political sphere when transferring scientific knowledge and what the most innovative trends in health are, among other things.
Both Panteli and Tille work on evidence-informed health policy and health care, focusing on the Observatory’s work pillar on innovation and its links to Health System Performance Assessment (Panteli) and cancer (Tille).
The Observatory is celebrating its 25th anniversary this year. What are the general insights of the organisation after so much time supporting and promoting scientific evidence to European health policymakers?
Dimitra Panteli: The first thing is the vast potential to learn from each other, that’s the whole point of the Observatory. The successes and failures that countries and organisations have had in trying to reform their health systems are lessons that can help others to improve and strengthen theirs.
Second, health systems are very complex: you may have ideas about how to change them, but whether you succeed depends on many factors, such as a good understanding of the systems or involving all the appropriate actors in the change process.
And third, health systems do not operate in a vacuum, but in an overall context, with other types of pressures to which they must be resilient. And these pressures are not always foreseeable and may come from outside the system, as we have seen with the COVID-19 pandemic or financial crisis.
Florian Tille: Context is indeed essential. Even if there is shared learning among systems, countries or regions, ultimately problems or challenges need to be specified and options for solutions tailored to the different places where you are trying to tackle these challenges. This dependency on the context is relevant for the provision of health services, for example.
What progress has been made in cross-border learning between EU Member States?
Dimitra Panteli: Obviously a lot, otherwise 25 years of Observatory efforts would have gone to waste! The European Union itself, with all its support for collaborative projects such as eCAN, is clearly moving in this direction. Proof of this is that its continued investment in this area has led to the emergence of various networks, initiatives and exchange platforms for boosting knowledge exchange across countries.
Initiatives such as Transforming Health and Care Systems Partnership (THCS) are trying to strengthen that collaboration by identifying what we need to look at and then promoting a common analysis.
Florian Tille: And if we talk specifically about cancer, the project ECHoS is also committed to create a European Network of Cancer Mission Hubs (NCMHs) that operates at national, regional and local levels. The Observatory is a key partner in this as we facilitate policy dialogues with the Mission Hubs.
Does the Observatory have any examples of such networks of its own?
Dimitra Panteli: We count on the Health Systems and Policy Monitor Network (HSPM). The knowledge of our experts is channelled through the HSPM platform, which provides detailed descriptions of health systems and up-to-date information on reforms and changes that are of particular policy relevance. This network, for example, was crucial during the pandemic as it provided information on how countries’ health systems responded to the COVID-19 between 2020 and early 2022 and the inputs to the COVID-19 Health System Response Monitor (HSRM).
The main gap between scientists and policymakers is the way information is presented and made accessible.
You mentioned earlier that it is important to involve the right actors. How do you get policymakers to listen to the evidence?
Dimitra Panteli: The main gap between scientists and policymakers is the way information is presented and made accessible. We often have good scientific studies on policy measures that are methodologically complicated or present their findings in a format without the “so what?” message that indicates their importance for legislators’ work. Therefore, there is a need for translation from scientific facts to feasible policy actions.
Really understanding how policymakers work, in terms of their needs and their own ways of operating, is a key ingredient for successfully transferring any insights from science to the political sphere. This is why the Observatory has both short-written formats and face to face formats, such as policy dialogues, to approach policymakers.
Florian Tille: The information overload we all face implies that we have to be much more specific, concise, and really intentional in our messaging. Not to mention that sometimes it is not the policymaker who works with our messages in the first place, but their closest advisor, so information is likely to pass from person to person. That’s also why the materials we develop have evolved in terms of framing and format: more multimedia, more compact formats, greater social media presence, etc.
Apart from the collaborative approach, what trends or innovations in healthcare are you currently observing in Europe?
Dimitra Panteli: I like to divide them into three categories, although they’re interrelated: there is the biomedical or technological innovation and then we also have the organisational innovation, which includes all the different models of care, for example.
There is a lot going on at the moment, so it’s hard to single things out – but perhaps we can provide some examples. In the first group, we have elements like artificial intelligence (AI) and health applications, with all the challenges that come with them: data privacy, cybersecurity, digital literacy, inequalities, etc. In the second group, we have the efforts done to deliver a closer care to patients without the need of visiting medical centres, such as “hospital at home”.
Of course, all this innovation means that professionals need to acquire new skills and we need to ensure that we can incorporate the innovations that really benefit patients in a way that is sustainable for the future.
Florian Tille: We also see innovation in long-term care. We’re just finalising a book on that topic. In one chapter we’ve taken a close look at the trend of more private providers entering this area (of long-term care), and what this implies for service delivery, costs, and most importantly, for the people receiving care, their families, and the workforce.
In the specific field of cancer, we are looking at the whole continuum of cancer care and research, focusing for example on things like survivorship and the ‘right to be forgotten’ for cancer survivors.
How is the process of consulting and selecting the scientific evidence and what types of sources do you use?
Florian Tille: In the Observatory, we do secondary data analysis, which means we consult the scientific knowledge that is in recent literature, and then we try to gather it to do our work. Always from an international or EU perspective.
And of course, we’re constantly talking to experts in different countries about what’s new, to get additional insights that might not be apparent from the literature at first glance. These networks are also useful when we need to respond quickly to requests from countries on different health topics that emerge all of a sudden.
Dimitra Panteli: Talking about quick responses, for example, a few years ago one European country asked us for help. They wanted to expand their dental coverage because they realised that their population had significant oral health problems. So, they asked what other countries had done to expand their basket of services in this area.
Behind these rapid responses, there’s a whole series of observations and country-by-country monitoring that tells us how health systems are evolving and performing and evolving, and then we can provide benchmarks by comparing them.
Policy dialogues, journals, webinars… the Observatory has many tools at its disposal to ensure that its message reaches policymakers. Which ones work best? Is there a need to develop other formats in the future?
Dimitra Panteli: They all have their uses! In general, if you look at the evolution of these formats, you’ll see that we used to do more long studies, and now we tend to use shorter formats like our policy briefs. As a technical advisor you should be able to highlight the key points that are needed in a simple way. To disseminate our written formats, we rely heavily on social media and try to present our points in different ways.
In the audiovisual format, we are also opting for short messages, although we are still experimenting and evaluating their use. We have suggestions for podcasts as well, but nothing concrete yet.
There are European elections next year. What do you expect from them in terms of health policies? Will there be specific health issues or challenges that, in your opinion, will set the tone for the next four years?
Florian Tille: The most immediate thing I can think of is the European Health Union (EHU), which is a very broad topic obviously, also pandemic preparedness and response and pharmaceutical pricing policies.
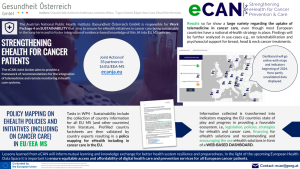
Dimitra Panteli: In fact, the European Commission has asked the Observatory to support with a public consultation on in which direction the health priorities should be moving forward. During the European Health Forum Gastein (EHFG) and the European Public Health Conference, the Observatory organised sessions about the future health priorities of the EU: such as strengthening and supporting the workforce, addressing the determinants of health, climate change and the sustainability of the health delivery system or the implementation of digital solutions and AI, to name a few. We will have additional webinars in January 2024 on these issues to engage with those who are interested. We will also continue working on topics from the current cycle as well, like the European Health Data Space (EHDS), for example.
EU projects must take advantage of windows of opportunity, because if they are not aligned with the political agenda, they will have a hard time achieving their objectives or generating impactful messages, no matter how good they are.
And one last thing that I think is important to mention, is that following the COVID-19 pandemic, there might be resistance to continue to focus and prioritise health over everything else when we have other areas that could use that money too. We already saw in this year’s State of the Union speech, is that there was very little discourse about health, so we need to keep making the case for investing in this area
There are several European projects, such as eCAN, that aim to produce general recommendations to help countries implement measures in certain health areas. How do you assess the interaction of these projects with the political spheres?
Dimitra Panteli: European projects are clearly moving towards a better understanding of the importance of communication and finding a way for their results to somehow land where they’re supposed to.
They must take advantage of windows of opportunity, because if they are not aligned with the political agenda, they will have a hard time achieving their objectives or generating impactful messages, no matter how good they are. eCAN is an example of how to take advantage of these windows, as it addresses two current key issues: digital health and cancer.
Florian Tille: Especially when it comes to disseminating and communicating key messages, it is absolutely essential to have a plan for the sustainability of the project and how your messages and findings will contribute to a meaningful change over time, because this is why the project has been commissioned in the first place. You have to think about how to promote the long-term impact of the initiative.
![]() Co-funded by the European Union. Views and opinions expressed are however those of the author(s) only and do not necessarily reflect those of the European Union or HaDEA. Neither the European Union nor the granting authority can be held responsible for them.
Co-funded by the European Union. Views and opinions expressed are however those of the author(s) only and do not necessarily reflect those of the European Union or HaDEA. Neither the European Union nor the granting authority can be held responsible for them.
 Pictures handed
Pictures handed
 The Photo Project
The Photo Project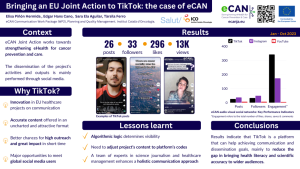
 Pexels (Thirdman)
Pexels (Thirdman)