The Steering Committee meeting of eCAN has been held today, May 11th, in a virtual format and with more than forty participants from beneficiary and affiliated entities. The meeting has served for the different Work Packages to present the progress achieved on the first quarter of 2023 and share their upcoming assignments.
The reunion has been welcomed by Matthias Schuppe, responsible for preparing DG SANTE’s work on the ‘Europe’s Beating Cancer Plan’, Maren Hunds, member from the European Health and Digital Executive Agency (HaDEA), Dheepa Rajan from the European Observatory on Health Systems and Policies and Caroline Berchet, health economist at the OECD Health Division. The four professionals have spoken at the beginning of the meeting, stressing the importance of the JA and the possibility of establishing synergies in the near future with other entities and European initiatives.
While all the Work Packages were able to share their progress, the bulk of this Steering Committee focused on the two pilots that eCAN is developing in teleconsultation and telemonitoring, which should be launched on June.
eCAN’s first achievements
Following the agenda, OECD and WHO/OBS, as eCAN observers, highlighted their supporting role to the overall project’s progress. The JA has been selected as example of project linked to quality of life in an exhibition of European projects organised by DG SANTE within the framework of the European Week Against Cancer (EWAC).
WP8’s presentation has been focused on stakeholders’ identification and engagement. The colleagues from Greece have organised and taught four workshops for eCAN participants between April and May. As for the upcoming tasks, WP8 will soon conduct a gap analysis and assess the training needs of patients, caregivers, and clinical experts. They will also develop an educational framework and training materials.
Andrea Pace, from the IRCCS Regina Elena Cancer Institute (IFO-IRE) has conducted both presentations of Teleconsultation (WP5) and Legal, ethical framework and cybersecurity (WP6), focused on the initial development of the JA’s pilots.
Halfway through the Steering Committee, the Telemonitoring team (WP7) has also given some insight into its work until now. This includes partially completing the landscape of remote surveillance of patients and the ongoing development of the telemonitoring system to start pilots testing. In fact, they show several mock-ups of the application that will be used to monitor patients participating in the study.
Progress on sustainability, evaluation and communication
The past and following months have also been addressed by the entities belonging to Austria, Poland and Spain, and they have discussed the risks, gaps and opportunities that they expect to experience in the upcoming weeks.
The Sustainability Work Package (WP4) has finalised all preparations on the Country Factsheets, documents that compile information on different territories’ preparedness, legislation and initiatives on cancer and digital health. They have been verifying the available data over the past months and country factsheets will soon be sent for external validation.
The team responsible for the Evaluation (WP3) is about to finalize the second progress report and is preparing the cost and consequence analysis framework together with the protocol for the SWOT analysis. Both milestones are scheduled for July 2023.
Finally, the Communication team (WP2) has presented their campaign for the European Week Against Cancer (EWAC) and showed the recent content published on the website (interviews, news, newsletters…) and social media, with TikTok emerging as one of the most prominent social networks for eCAN. The Spanish team has already submitted two deliverables, the most recent one being the updated version of the Communication and Dissemination Plan. The main ahead tasks for the communication team include preparing the first Annual Report and start organising the project’s final conference.
Towards the first half of the Joint Action
The Joint Action “Strengthening eHealth including telemedicine and remote monitoring for health care systems for cancer prevention and care”, launched in September 2022, is approaching its first year.
The summer months will be crucial for its progress and evolution, as many important milestones will be reached, with the start of the pilots being the most important one. At the same time, the first anniversary of eCAN will also serve to take stock of what has been achieved so far and to preview the outcomes that this European initiative could provide. Such progress will be monitored and explained in more detail at the next Steering Committees.
![]() Co-funded by the European Union. Views and opinions expressed are however those of the author(s) only and do not necessarily reflect those of the European Union or HaDEA. Neither the European Union nor the granting authority can be held responsible for them.
Co-funded by the European Union. Views and opinions expressed are however those of the author(s) only and do not necessarily reflect those of the European Union or HaDEA. Neither the European Union nor the granting authority can be held responsible for them.

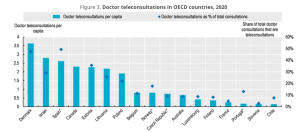
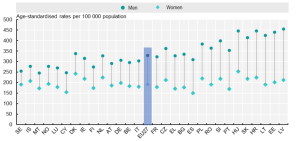
 OECD
OECD