Equity and digital transformation are not always perceived as two sides of the same coin, and although there is an undeniable change in how we behave and interact in this technologically driven World; it is not less true that digital tools offer an incredible range of innovative solutions that can be helpful to reduce inequalities in different fields.
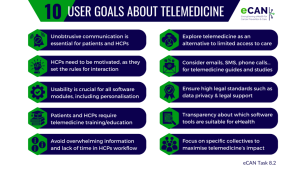
The transformation healthcare systems are undergoing is intrinsically linked to the incorporation of digital solutions. But there are still some doubts on how this should be done, and the fact that research shows that telemedicine can close healthcare gaps is not enough to fully embrace digitalisation yet.
In the specific field of cancer, research efforts are focused on consolidating telemedicine as a common practice across Europe, enabling equal access to care. The current scenario reveals that there are gaps in cancer care depending on where the cancer patient lives, whether urban or rural areas; their socio-economic status; the population group they belong to; and how they identify. These are what we know as social determinants of health.
Inequalities based on our ZIP code
15500 and 06240 are ZIP codes from Fene (north-west Spain) and Sjøholt (west Norwegian coast). Despite being 2320 km apart, these two villages have something in common: both are rural areas where access to cancer care differs from the one in big cities. Mónica Fernández, from Spain, and Nils Petters Sjøholt, from Norway, as cancer survivors, know that for a fact. They are well aware that when cancer touches someone’s life in these territories, distances become problematic, since patients often need to travel long distances to have access to treatment, psychological support and rehabilitation processes. According to Mónica, “living in a rural area ensures quality of life, but healthcare services close to my place should be better equipped”. She was diagnosed with breast cancer in 2021 and had to travel 40 km to receive radiotherapy for three months, “although there are people from my region that need to drive up to 100 km to get the same treatment”, she adds.
Nils Petters’ experience has some resemblances. When he was first diagnosed with prostate cancer in 2003, he had to go to Trondheim to get surgery, 260 km from his hometown. “For three years I went to Trondheim for control visits every three months”, he explains. Later on, when he was diagnosed with appendix and skin cancer, he received his treatments a little bit closer, 40 km from Sjøholt. “People living in an urban area have things easier”, he points out.
The evidence supports his statement. Several studies on cancer care and inequities reveal that cancer patients living in rural areas experience health care disparities and poorer clinical outcomes than their counterparts in urban areas. One useful fact to understand where these inequalities come from is that the “average road distance to essential services is much shorter in urban areas compared to rural areas”, according to EU data, and that may affect almost 1 out of 3 people who live in the countryside in the European Union. For instance, in remote rural areas, the average road distance to the nearest doctor is almost 21.5 km, compared to 3.5 km for people living in cities.
In this sense, Vittorio Castaldo, project manager of the eCAN pilot projects and researcher at the Regina Elena National Cancer Institute in Rome, states that the greater the distance and the travel time, the higher the chances of neglecting patients’ needs. Offering continuous monitoring and psychological support through digital tools “empowers patients and helps us to ensure that patients who live far from medical centres receive equal care than those who live in urban areas”, Castaldo adds.
A network of support
Neither Mónica nor Nils Petters received psychological support. In her case, Mónica did not apply for it, although she thought about it. “When I got my diagnosis, I did not react well. I knew I had a lump, because I could touch it, but after tests, they found five lumps. Doctors finally decided that surgery was the best way to tackle it, which was not my preferred option. That was when I felt the World was falling apart”, she explains.
Thanks to her family and friends’ support, and also because “cancer was never a taboo” for her, she could mentally deal with it. However, she stands for “providing psychological support to everyone who needs it. Cancer processes are not the same for everybody and depending on the sequelae, patients may or may not require it. In my case, I was a young woman who also did not suffer so many corporal changes. When your physical appearance changes a lot, I think it is harder”.
When Nils Petters recounts this period of his life, he relies on humour. “They [doctors] used to remove small pieces of my body from time to time”, he explains while laughing. For him there is a paradoxical truth: “the key to fully recovery from cancer lies in early detection”. In the case of prostate cancer, active surveillance and the use of the appropriate early detection tools can make a big difference in the possible outcomes of a patient.
In this case, Nils’ wife was his psychological support, because by that time it was overwhelming to find this kind of help and reliable information in public services. He acknowledges the importance of providing psychological support “to anybody with a cancer diagnosis, especially after treatment”. However, accessing these services is not always easy. “If you need a therapist, you have to go to your regular doctor, and s/he needs to apply for it. When I was a patient, it was not certain that you’d get it, and there was a long waiting list because there was and still is a workforce shortage”, he points out.
Neither of them has used telemedicine services, but both agree that if they had had the chance to use digital tools, they would have tried them. Mónica notes that “digital tools and communication are paramount, but you also need patients to have some digital literacy”. Nils Petters believes that it would have been much easier for him to have had these tools at that time.
The role of telemedicine
In fact, technology transforms the way patients face cancer. “Distances become shorter”, says Efthyvoulos Kyriacou, the head of the Telemonitoring team at eCAN that works at the Cyprus University of Technology (CUT). “A patient might need to talk to his or her physician or psychologist and thanks to telemedicine they do not need to wait three weeks for an appointment. You can have that on a more regular basis through telemedicine services”. Digital tools enable communication, and the opportunity to connect the right clinician to a patient, instead of moving the patient around. “This is especially relevant for countries that have dispersed population in large rural areas”, argues the CUT’s professor.
At eCAN, research efforts are dedicated to developing mobile apps, web-based interventions or the use of wearables for remote monitoring of pain, anxiety or quality of life. According to Kyriacou, it was after COVID pandemic when “the healthcare community started appreciating the opportunities and usefulness of tele-support and telemonitoring, perhaps also because new generations are digital natives”.
His perspective coincides with Castaldo’s view. The Italian expert believes that “opening up this new scenario for telemedicine is useful to create a more sustainable and effective healthcare era”. However, “it is relevant to keep in mind that telemedicine is not replacing in-person visits, rather it is a parallel tool useful to overcome some issues related to cost-effectiveness and remote access to care”, he concludes.
Navigating paths towards equality: where to focus?
As is often the case, innovation outpaces legislation. Digital tools are available, but the legislation enabling their operation is yet to catch up. However, it appears to be closer than ever. After years of documents bouncing from one institutional desk to another, the prospects of finally reaching an agreement on a European Health Data Space (EHDS) are promising.
“The EHDS will be the pillar that sustain health data management, and the guide that defines how the General Data Protection Regulation (GDPR) should be handled across the European Union”, Kyriacou explains. The document is grounded in the 2022 proposals of the European Commission, and both the Parliament and the Council have reached their own views on what the final text should contain. The two are now entering negotiations with each other, involving the Commission as well, with the aim of reaching a final agreement that can be enacted into law.
Integrating digital tools into clinicians and patients’ daily routine is also a matter of persuasion and trust-building process. During the recruitment phase for the eCAN pilot projects, Vittorio Castaldo has seen both negative and positive reactions. Whereas some patients feel reluctant to use it because they “want to have this eye-to-eye conversation with the clinicians, to catch their gestures, etc.”; there are others that “are happy to receive tele-rehabilitation care for breast, and head and neck cancer, and mainly tele-psychological support”. In the trust-building process, Mónica Fernández also highlights the importance of “mastering the art of communication”. “Healthcare professionals need to learn how to better explain what is happening to us and encourage us to get psychological support. They cannot force us, but they can stimulate us”, she points out.
Digital tools are available, EU regulations are on their way and the ability to convey the right message to the proper actors is a never-ending task. Navigating the journey towards equitable access to healthcare presents ongoing challenges, not only in the realm of cancer care but also in its prevention. What seems to be unmistakably evident in this intricate process is the growing influence of telemedicine, now asserting its position in the core of European healthcare systems, akin to a respected member at the family dining table.
 Co-funded by the European Union. Views and opinions expressed are however those of the author(s) only and do not necessarily reflect those of the European Union or HaDEA. Neither the European Union nor the granting authority can be held responsible for them.
Co-funded by the European Union. Views and opinions expressed are however those of the author(s) only and do not necessarily reflect those of the European Union or HaDEA. Neither the European Union nor the granting authority can be held responsible for them.

 eCAN
eCAN