INTERVIEW
There are high expectations that digital tools can contribute to a lower incidence of cancer, although we are still testing and evaluating many of them. What is certain, however, is that technology will not be enough if we do not change our lifestyle habits. We have already heard this with climate change, with the energy crisis, with our consumption patterns… and cancer is no stranger to this.
This idea is also advocated, among others, by Wendy Yared, Director of the Association of European Cancer Leagues (ECL) with more than 25 years of experience in public health and health policy. The organisation she leads brings together national and regional cancer societies that cooperate and exchange information to curb the impact of cancer at European level.
Question: In Europe, we are making great efforts to reduce the incidence of cancer, but how can we do even more?
Answer: We need to put more emphasis on cancer prevention so that we can save more lives. I am always surprised that many people are still not aware that up to 50% of all cancers are preventable. This means that not all cancers are inevitable, and we need to encourage everyone to understand it.
Why have not we paid more attention to prevention until now?
Only 3%, or even less, of health budgets are devoted to prevention. And I am not just talking about cancer prevention, but about prevention in general. When there are few resources and attention, there are not enough actions to reduce the incidence of these diseases.
Moreover, cancer takes decades to develop, so if there is a current improvement in its incidence, it is due to the efforts that were made decades ago. Maybe what we are doing now is very good and sufficient, but we will not be able to see numbers improve significantly for another twenty or thirty years. The good news is that now, at the EU level, there is a lot more attention towards cancer control and policymakers are being convinced about of its importance.
Considering the available data about the growing incidence of cancer, how is ECL looking at the future?
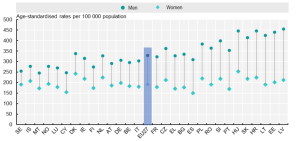
First, it is important to know how reliable the data and the sources are, but it is certain that the ageing of Europeans plays an important role. For our part, we are trying to maintain cancer high on the EU agenda, because this has not always been the case.
We must be patient, but there are reasons for hope, such as increased budgets for cancer control and a bigger awareness in Europe. I am confident that we will see a decrease in cancer incidence soon, especially with the increased EU support in recent years.
“I am confident that we will see a decrease in cancer incidence soon, especially with the increased EU support in recent years”.
Nowadays, it is known that our habits and the risk of suffering cancer are linked. Why is it so difficult to raise awareness of this idea among people?
Each risk factor responds to specific behaviours and, as a result, there are different challenges in each of them. For some risk factors, such as tobacco use, we have more information on why it is so hard to modify our habits, but we also know actions that work, such as taxation. If there are high prices, it will be more difficult for people, especially youth, to get hooked.
Cancer leagues need the support of governments to improve policies and raise awareness, considering that we do our best with fewer resources than industry, which widely promotes its unhealthy products (tobacco, alcohol, sugary drinks, sunbeds, etc.).
How can we convince them to lead healthier lifestyles?
The International Agency for Research on Cancer (IARC) is now in the process of updating the European Code Against Cancer. They are evaluating what works and what does not in each cancer area while considering the most updated evidence. It is important to keep renewing the messages regularly so that people are reminded of them. And finally, as mentioned before, it is important to have policies that encourage citizens to make the healthiest choices.
Can you give us some insight into the upcoming fifth version of the European Code Against Cancer and how do you plan to increase its dissemination?
There will likely be new recommendations that will be added to the current fourth edition. Discussions are ongoing to align with current evidence, such as including boys for the Human Papilloma Virus (HPV) vaccinations.
Regarding the dissemination, we will continue to engage the member leagues of the ECL and other partner international organisations to spread the word about the ECAC, since they have direct contact with patients and civil society.
The ECAC and other initiatives focus on what we can do as individuals to reduce cancer risks, but do we ask the same commitment from producers (alcohol and tobacco companies, food industry…)?
We can ask but I have little confidence that they will have any significant level of commitment. While some companies may show that they try to make a difference, not all of them do what they promise. It is simple: it is not their job and they want to sell and make a profit. We have different priorities and that forces us to seek a balance between all the actors involved.
If producers truly wish to help, they could give a portion of their profit to support healthcare systems, because if they are going to make people sick, at least help them get better too.
“While some companies may show that they try to make a difference to reduce cancer incidence, not all of them do what they promise. It is simple: it is not their job and they want to sell and make a profit”.
In terms of digital tools for cancer care, it is very common to mention mobile apps, but can you give other examples of these tools? Is there one that stands out above the rest?
When we talk about digital tools, we also include smartwatches, the Internet of Things, robotic surgery, pathologists… but none of them stand out among the other tools for now. We have to wait for the results that all of them are promising and bringing. The internet and websites, if we count them as digital tools, are the most promising because of their accessibility, durability and reach.
How can digital tools help us to deliver cancer services more efficiently and reduce existing gaps?
The patient must be well-informed to be able to choose which option he or she prefers and to have flexibility in this regard. Beyond highlighting the benefits of these tools, such as reduced travel time and the guarantee that the doctor is always there, even if not physically, what is really important is to give the patient the possibility to choose between virtual or face-to-face care for their particular needs.
What are the barriers that healthcare professionals need to overcome?
The pandemic has shown that there is a new way of working in healthcare and has helped professionals change their mind-set on the value of digital health. Not everyone was trained with these technologies when they were studying, like surgeons, for example, so their learning curve has been steep and fast. They also have had to learn how to talk to patients through the screen when there are difficult things to tell. Professionals need to be convinced that this adaptation can be useful to them and make their work easier.
And regarding the management of health information?
Hospitals use different systems to manage their data, so harmonisation of information and platforms across healthcare institutions remains a challenge. We need to ensure that these systems are interoperable within and across our borders.
Patients can be nervous about sharing their data, because sensitive information can be grounds for discrimination if it gets out or is leaked, so these systems need to be secure and the patient needs to be assured of the confidentiality of their information.
What added value can eCAN bring in the context of digital tools?
eCAN aims to put on the table some recommendations on teleconsultation and telemonitoring at European level, which I believe is vital to clear up doubts and ensure that everyone interprets the regulations in a harmonised way. But for this to happen, it is first necessary to raise awareness among policymakers, which is also what eCAN is trying to do.
![]() Co-funded by the European Union. Views and opinions expressed are however those of the author(s) only and do not necessarily reflect those of the European Union or HaDEA. Neither the European Union nor the granting authority can be held responsible for them.
Co-funded by the European Union. Views and opinions expressed are however those of the author(s) only and do not necessarily reflect those of the European Union or HaDEA. Neither the European Union nor the granting authority can be held responsible for them.
 OECD
OECD