Effective communication, training and support: key elements for the smooth adoption of telemedicine
As a Joint Action aimed at reducing inequalities in cancer prevention and care, end-user perspectives and reflections are central to eCAN. The INAB|CERTH organisation has undertaken several actions under Work Package 8 to actively involve potential end-users and gain a comprehensive understanding of their perspectives on eHealth services. This involvement has led to the organisation of three focus groups under the task 8.2, Participatory Design, in which members of AUTh and 3rd RHA have also participated.
The first focus group (FG) focused on exploring participants’ perceptions of telemedicine and involved thirteen participants (patients, healthcare professionals and patient support workers). In the second, five patients participated to give their opinion on the eCAN mobile application while in the third healthcare professionals commented on the dashboard platform. Taken together, these discussions have provided important input from the wide range of participants involved.
Key points from the eCAN focus groups
The findings from the telehealth focus group highlight many challenges and needs of patients, HCPs and patient supporters. Effective communication, education and support emerge as critical elements for the smooth adoption of telemedicine.
In terms of the technologies that are being developed, the focus group discussions highlight specific requirements and considerations. For the eCAN app, patients expressed satisfaction and provided valuable suggestions, emphasising the importance of usability, improved data visualisation and additional features such as calendar functionality.
On the other hand, discussions on the eCAN dashboard revealed insights from HCPs, emphasising the need for adaptability, immediate technical support and the potential use of the dashboard as a complementary tool to regular care.
The conclusions from the telehealth focus groups are consistent with the technology-focused discussions developed, highlighting the importance of user-friendly design, immediate support and clear demonstration of benefits to both collectives. Bridging these aspects is crucial for the successful integration of telemedicine technologies into healthcare systems.
End-users’ perspectives on telemedicine
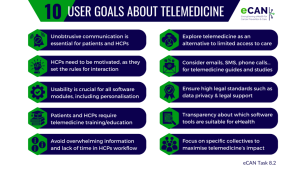
The results of the first focus group, focused on telemedicine, are summarised in ten user goals. These include elements such as non-intrusive communication, which is crucial for the interaction between patients and healthcare professionals, and increased motivation for the clinicians as they set the ‘rules’ for such communication.
Usability has been also identified as a relevant step for all software modules, including personalisation capabilities. At the same time, the need for more digital literacy training for patients and professionals and a commitment to short and concise interactions is also emphasised.
Telemedicine is emerging as an alternative for cancer treatment and monitoring, especially in rural areas where patients have limited access to healthcare providers. However, in addition to the use of mobile applications and instant messaging, it is concluded that more mature and less intrusive means of communication (e.g. email, SMS, phone calls, etc.) should also be actively investigated as part of practical telemedicine guidelines and/or pilot studies.
Of course, as these virtual alternatives are developed, the implementation of strict regulations should not be neglected, including the protection of patient data and legal support for healthcare professionals in the event of an error. To ensure trust, there should be transparency about which software tools are suitable for use in the eHealth context, perhaps through well-known certification schemes.
Finally, focusing on specific population groups (e.g. people with limited mobility, minorities with limited access to health services, or younger people who would be more likely to adopt eHealth tools) is crucial to maximise the impact of telemedicine services, reduce their risk of adoption and improve the risk-benefit ratio.
User Goals about telemedicine
Insights about the eCAN mobile application and the dashboard
In the other two focus groups, both patients and healthcare professionals have also provided different insights on the eCAN application and the dashboard platform, respectively.
Participants in the first group stressed the need to involve people with different levels of digital literacy in usability studies and to visualise information or data beyond numbers for better interpretation.
On the other hand, patients’ concerns arise when the use of such applications may lead to a deterioration in their health status and exacerbate the impact on their mental health. They also argue that the benefits of using the app should be clear to both patients and healthcare professionals.
In relation to the dashboard, clinicians comment that the platform used for eCAN needs to be resilient to emerging needs in clinical practice and provide immediate technical support during its operation. “Guidance from people who have used the platform in practice would also be helpful”, they have said.
They also point out that the dashboard could be used as a complementary tool to routine care and should be designed to fit the workflow of each healthcare professional, increasing the usefulness of primary data to improve patient care.
Reference
Active Involvement of Potential End Users in Strengthening eHealth for Cancer Prevention and Care (WP8). 2024.
![]() Co-funded by the European Union. Views and opinions expressed are however those of the author(s) only and do not necessarily reflect those of the European Union or HaDEA. Neither the European Union nor the granting authority can be held responsible for them.
Co-funded by the European Union. Views and opinions expressed are however those of the author(s) only and do not necessarily reflect those of the European Union or HaDEA. Neither the European Union nor the granting authority can be held responsible for them.